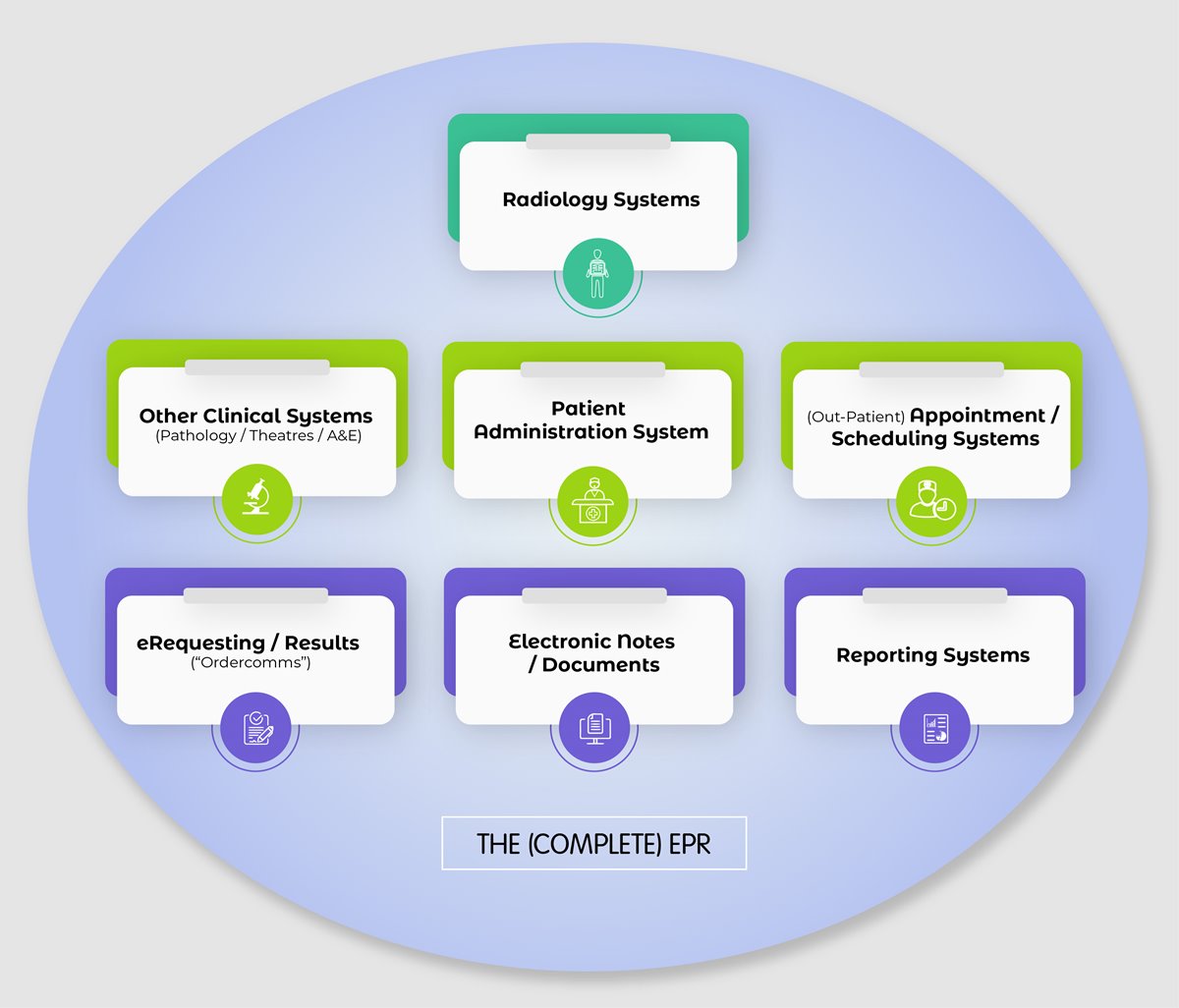
The EPR is a method of storing medical records and notes electronically rather than in bound paper bundles, thus allowing the effective accessing and sharing of data. EPRs should encompass the entire digital record ecosystem rather than just refer to the standalone viewer application.
Systems within the EPR Ecosystem
We’re all familiar with PACS and RIS. These two stalwarts can be supported by a number of additional functions or integrations depending on local need:
Voice or Speech Recognition / Digital Dictation (for faster transcription of reports);
eRequesting (ordercomms) for electronic requesting (to standardise and streamline referral processes);
Data Analysis Software (to generate reports such as activity and demand);
Billing systems (a key part of private sector imaging centres cost management);
Abnormality flagging systems (to automate unexpected finding processes and ongoing care);
Result systems (usually to feed back to GPs ordercomms);
Data Sharing services (within the NHS typically the Image Exchange Portal for cross-organisational patient care);
National databases (such as the NHS Spine for patient demographics and national Numbers);
Patient management systems that have access to all clinic lists, patient location etc. (more commonly found in the private sector);
Standalone systems for wider clinical areas such as Radiotherapy, Nuclear medicine, Obstetrics, Neurology, Cardiology etc. may also be linked.
On top of these, a shared Master Patient Index (or “Patient Administration System”) provides patient demographics (name, address, date of birth etc.) and feeds into most of the systems.
An EPR takes information feeds from the departmental systems and can provide information from its enterprise-wide components such as scheduling. It can function simply as a digital librarian bringing together demographics and the various patient contacts within the hospital and also provide complex functionality such as logic (gender, age) specific to the pathway a patient may follow (See diagram: The Complete EPR).
What does an EPR Do?
An EPR is a data presentation system replacing the need to collate paper bundles. Subject to security permissions, the electronic information can be updated and accessed in real time by a range of end-user devices connected to the system almost as easily as if they were paper based.
For patient care in radiology this could provide useful information from surrounding services such as:
View a list of upcoming procedures requiring image intensifiers in theatre (better planning, resource allocation and reducing ‘surprise requests’ for screening);
Scheduling patient appointments to synchronise (or not clash) with a patient’s other Outpatient Department attendance or diagnostic investigation;
Verifying laboratory results or requesting a test be performed prior to CT biopsy and other studies from a connected Laboratory Information Management Systems (LIMS);
Checking patient status and location before sending a porter to bring the patient to imaging.
Main Types of EPR
- The All‐In‐One
This type of EPR uses software derived from one single supplier for the whole system. Common suppliers in the UK are Allscripts, Cerner, DXC, IMS Maxims, Nervecentre, Meditech, TPP and System C - all accredited suppliers for NHS England. Having one supplier allows most of the modules to generally ‘talk to each other’ very well, as all functions run on a common framework.
2. Best of Breed
This is a very popular contrasting approach with the involvement of different suppliers. In this approach, one company or the Trust may supply the Patient Administration System, and various other specialist companies provide imaging, A&E or therapy systems.
Best of Breed solutions will normally have an integration engine which all the modules have to communicate through (this links them up). The Integration Engine receives information from one module and can send it on to another (a GP request can go through the Integration Engine to the RIS and also to the main components of the EPR, perhaps stating a request is pending, for all staff to see). As the Best of Breed solutions have numerous companies looking after the various modules there is a risk of the ‘buck being passed’ when issues are found and a greater burden on system managers to implement good control.
Currently, staff may need multiple usernames and passwords to access the various modules - these are not true EPRs. There may be workarounds in place however - some Trusts use smartcards or Single Sign On applications, where another piece of software allows staff to securely authenticate onto multiple applications and websites (potentially automatically when they are opened or clicked onto), which saves time for the user.
There are documented advantages and disadvantages with both approaches. Many Trusts in the UK chose to adopt the Best of Breed model. There are some Trusts that have developed their own EPRs, which have modules from other suppliers bolted on. The term EPR does technically refer to the entire ecosystem including all the ‘local clinical’ systems.

Anant Patel (right): ‘An EPR is a data presentation system that replaces paper bundles. Subject to security permissions, the information can be accessed in real time’
EPR Implementation
Moving to digital storage does not have to be a slow process if resourced and implemented following project management methodologies, though there are some issues to be aware of:
Training on a new system - up to 15,000 staff (after Trust mergers) may need to be trained on their components of the system. Initial training is often executed well. However, when agency, bank or permanent staff need training later there may be gaps depending on which person is delivering the training (professional trainers or existing staff may not pass on all the information necessary);
Activity or data reports may need to be extracted by non-radiology staff, as information analysts may be required to use certain tools to run reports;
Staff may not like the system, believing it requires too much data input. However, if the whole system goes down and staff were unable to access the information, they would soon realise the benefits of an EPR. The sudden lack of information would require extra resources to revert to paper or spreadsheets until the system is restored.
Beyond the EPR
The next level up from the EPR is the Electronic Healthcare Record (EHR) which conceptually builds a patient’s record from the cradle to the grave. An EHR is a combination of systems (GP, community, mental, sexual and offender care systems) that can communicate data with EPRs and vice versa. The EHR allows the EPR to communicate information with other systems, going beyond traditional organisational boundaries.
Currently there might only be read-only interactions with the other local clinical systems, although standards such Fast Healthcare Interoperability Resources (FHIR) will enable information to be exchanged.
Further information on the interconnections, including flow diagrams, can be found in Chapter 6 of Clark’s Essential PACS, RIS & Imaging Informatics.