Do you ever wonder how a patient gets from A to B and what is involved? All the patients that come through the doors of an imaging department will be following a patient pathway, some of these are very short whilst others are a “long and winding road” with many twists and turns.
I am sure that all of you can think of many different patient pathways that you come across in your daily work, some are confined to imaging only whilst others involve complex integration with other departments.
As a radiographer you may only be aware of the small part of the patient pathway which is relevant to you and your interaction with the patient and are not sure what happens next in the pathway. But do you think it would improve the patient care if you did know what was happening next and you could discuss this with the patient? Maybe if we understood the “longer road” we could improve it and maybe even shorten it.
Patient pathways
Within the QSI we talk a lot about patient pathways, and it is often highlighted as an area of improvement for services as they start their QSI journey. It’s not that services don’t have pathways in place, its more that they aren’t formally documented and therefore how do we know what they involve. Services working on or already accredited will need to provide evidence of these, some examples from the standard are pathway and condition protocols and how these are managed, that plans are in place to ensure staffing requirements and the availability of equipment are met to avoid impact on the patient pathway. As part of the accreditation process, services will need to demonstrate, for each standard statement, that they have a ‘system in place’ and
- How does everyone know about your system?
- How do you know everyone is working to the system?
- How do you know that you couldn’t have a better system?
How can you do this?
You can start very easily by choosing a patient pathway, maybe it’s a new one or a well-established one which isn't working as well as you think it can. Start by creating a process map that will provide you with a visualisation of how the pathway currently works, you can see who and what is involved in each part of the pathway. This should help you identify any areas of waste or duplication and will also highlight where you have got it right.
You can then use these parts of the pathway to support other pathways. A process map should be updated as you continue to improve your process.
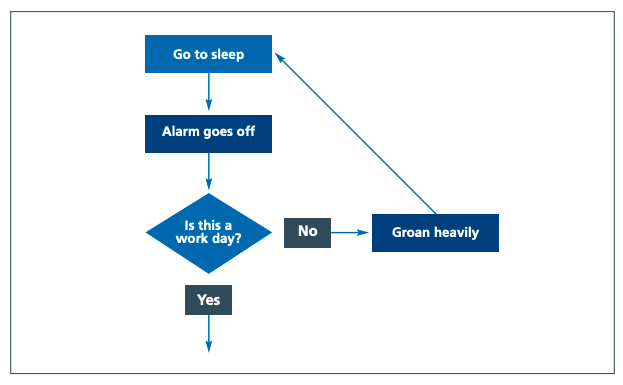
Your process maps don’t need to be complicated, a simple process map taken from NHSI conventional mapping process shows the steps for getting up in the morning, with boxes representing the activities and a diamond for a decision.
One of the biggest challenges when looking at your processes is getting the right people together to identify each step of the process you want to review and getting the time to do it. Making a small change in a pathway which works for you may have very different consequences in a different part of the pathway, to either another service or to patient care.
So, make sure you review any changes to make sure they are better for all concerned.
Helpful tips
- Where possible, create process maps with Post-it notes. People will feel more comfortable making changes to this, increasing the chance that your map will be accurate
- Ensure that you have everyone who is involved in the process present when you create the process map. This will allow for discussions about all parts of the process, including parts people might do differently or who are not part of the imaging service
- If you can’t have everyone present, consider starting the map and then leaving it in a shared space (e.g., staff room) where people can look at it and make changes to it
- When making the map, keep it visible to everyone so that all team members can see what is being suggested
- Once you have a map that people agree on, look for any duplication, any ‘dead ends’ or any steps that don’t add value. Consider focusing your improvements in these areas
- Discuss the parts that people do differently. It may be important to start with reducing variation in these parts of the process before starting other change ideas
- Agree on the beginning and end point before starting your process map
- Consider having a patient look over your process map to check whether your understanding of what they experience is correct.
Challenging the way that things are done can often be difficult and met with resistance, but unless we sometimes make that decision and challenge ourselves, we don’t know if a process can be improved.
If you would like to know more about QSI then contact the QIP at [email protected] for a chat and we can introduce you to the QSI network which offers support and knowledge to anyone who might be interested in learning more.

