I am a diagnostic radiographer by background, and after spending 10 years working in clinical practice, have worked in higher education teaching student radiographers since 2006. I developed an interest in person centred approaches to care whilst carrying out some research as part of my Masters in Education.
This led to me undertaking a large-scale national research project to define informed measures of patient centred care in diagnostic radiography as part of my PhD. In autumn 2021 I was appointed as the clinical director of the Personalised Care Institute, based on my PhD research and subsequent post-doctoral work on person centred care and personalised care.
Personal experience
On a personal level, I have had insight into the importance of personalised care. When my mother-in-law was diagnosed with a large Glioblastoma in 2018, as a family, we were left reeling with the diagnosis, and coming to terms with the knowledge that even with all the treatment planned for her (surgery, radiotherapy, and chemotherapy), we possibly only had a year left with her.
Throughout her illness, my mother-in-law had repeated interactions with both diagnostic and therapeutic radiographers, mould room technicians, oncologists, and a variety of other health care professionals. Most of those experiences were truly person centred, shared decision making and personalised care and support planning was evident. Like the findings of my PhD research project, little things made a big difference to her.
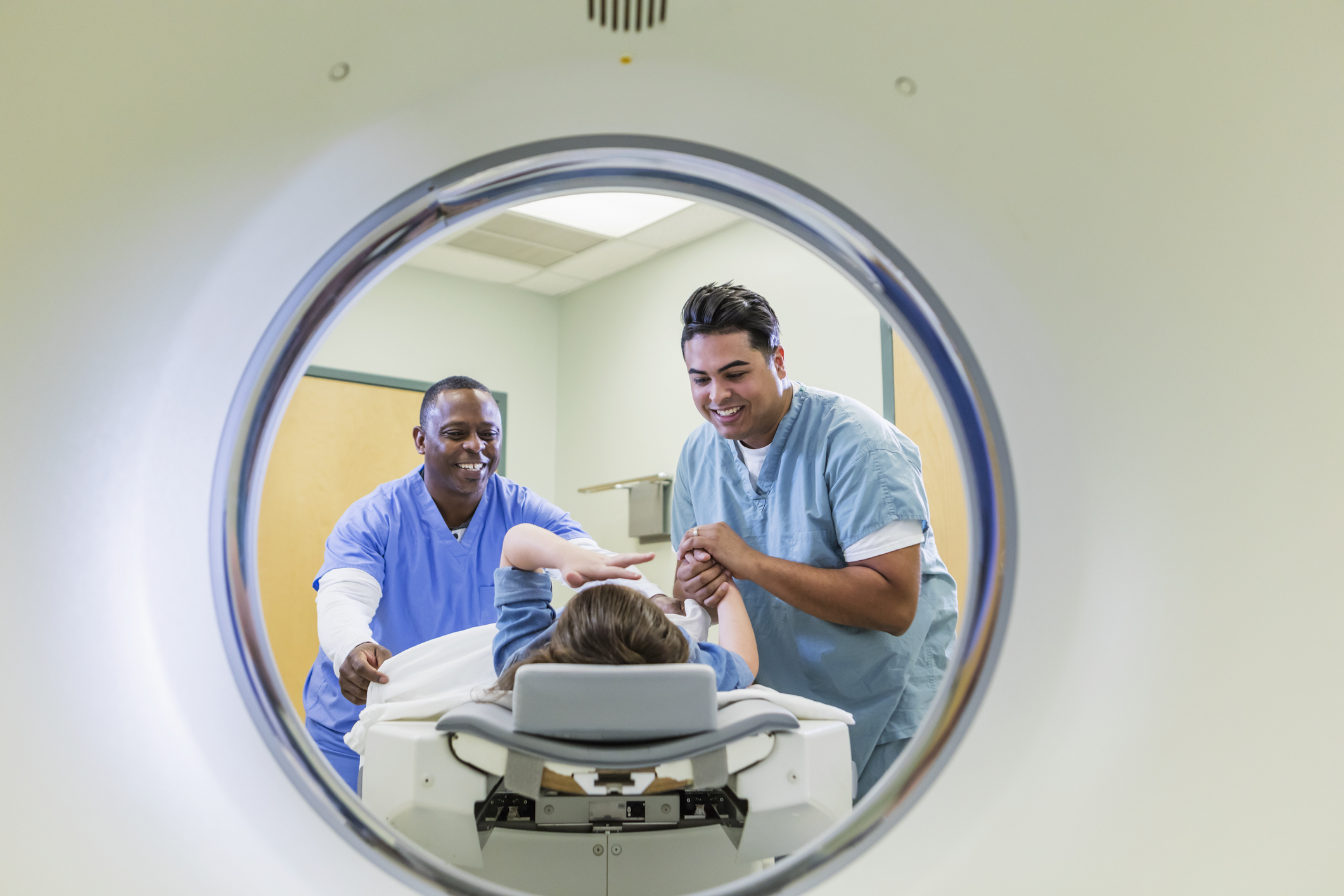
Being provided with a blanket to keep warm during an MRI scan, being allowed to take a family member into the radiotherapy mask fitting or the MRI scanner to hold her hand, and conversations about the weather or what had happened on the latest episode of ‘Escape to the Chateau’, not just her illness, made an enormous difference to her.
Extra pillows and positioning aids helped to make her more comfortable, particularly when her legs became swollen and ulcerated due to the steroids, she was ironically taking to reduce the swelling around the tumour. None of these acts of kindness were expensive or complicated, but they made an enormous difference to her feeling cared for. And as a family, we appreciated our inclusion in shared decision-making conversations and care planning.
Work to do
In my role as clinical director of the Personalised Care Institute I have realised how far ahead many radiographers and sonographers are in terms of knowledge and application of personalised care approaches. However, there is still work to do in some areas to raise awareness of personalised care, and increase the numbers of health and care professionals trained in personalised care, to meet the targets set out in the NHS Long Term Plan (2019).
Excellent CPD
The Personalised Care Institute supports the health and care workforce to deliver personalised care by providing FREE, quality assured education, training, and resources. We offer several e-Learning courses in areas such as shared decision making, personalised care and support planning and remote consultations. We also run regular live webinars on a range of topics such as long-term mental health conditions and social prescribing, and have a podcast series about topics such as long COVID and veteran’s health. All of which is excellent CPD! If you would like to find out more, please visit our website at: https://www.personalisedcareinstitute.org.uk/