The negative impact Covid-19 has made on cancer services has been reported widely in the media. GPs have seen a reduction in patients presenting with suspected cancers, screening services have been paused and investigation appointments have been cancelled or delayed1. What has not been reported are the positive changes that have been implemented in departments across the country in response to the unique pressures presented by the pandemic.
In Leeds, these new ways of working have contributed to the speed of project delivery. Remote working has enabled staff to work more flexibly and have productive and efficient meetings while minimising face-to-face contact.
In May 2020, a new radiotherapy treatment technique was implemented for breast patients just three days after trial results supporting the change were published.
Introduction of five fraction breast treatments
The Fast Forward Trial group looked at the efficacy and late normal tissue effects of hypo fractionated radiotherapy; comparing three weeks of treatment with just one2. The five-year results of the study were published on 28 April 2020, showing that giving 26Gy in five fractions over one week is non-inferior to the previous UK standard treatment of 40Gy in 15 fractions over three weeks.
The opportunity to provide the same oncological outcome while minimising hospital visits and potential Covid-19 exposure for these patients was seized upon. The pandemic provided the push that was needed to introduce the new regimen quickly so as to reduce hospital visits for these patients from 15 to five.
A multidisciplinary team for the project had been set up in March 2020 in anticipation of the publication of the results. This ensured the department could implement the changes as soon as the trial reported. The first patient was treated in Leeds with the new hypo fractionated regimen on 1 May. Although a quick introduction was needed, patient safety is the top priority so the standard procedures still had to be followed and the new protocols evaluated (Figure 1, below).
Verification
As the planning technique was to remain unchanged, it was decided that the standard treatment verification technique was still suitable (kV/MV pair), but as there would be a higher dose per fraction, the imaging frequency was changed to daily online imaging. An advanced practitioner was present for the first five patients to highlight
to radiographers the necessity to investigate problem set-ups before treatment delivery, for example, rotation or
contour change.
Treatment delivery
The actual treatment delivery process had no changes from the standard protocol. In order for the radiographers to become accustomed to the new daily imaging schedule, it was decided that the first 10 patients should be free breathing, only to remove the added complexity of voluntary deep inspiration breath hold (vDIBH). It was then opened out to any patients fitting the hypo fractionated treatment criteria.
Treatment review
A novel approach was needed for the treatment review of the hypo fractionated patients. At Leeds, the RTOG (Radiation Therapy Oncology Group)3 grading tool is used to assess skin reaction. Standard 15 fraction breast patients have a radiographer-led skin assessment on their last day and any patient with RTOG 2.5 or above would be referred for a nurse review along with any patients that would benefit from nurse review regardless of RTOG.
Due to the shorter treatment course, hypo fractionated patients were not expected to experience side effects while on treatment. Brunt et al (2016)4showed that if a patient in the 26Gy in five fraction patient cohort was to experience a CTCAE (Common Terminology Criteria for Adverse Events) Grade 2+, it would likely occur two weeks after starting radiotherapy. It was decided, therefore, that a nurse would perform a telephone review at 10 days post completion of radiotherapy, using a new assessment form. The form recorded bra size, the patient reported RTOG toxicity score, other skin conditions, current skin care and whether they needed further intervention (nurse-led or clinician).
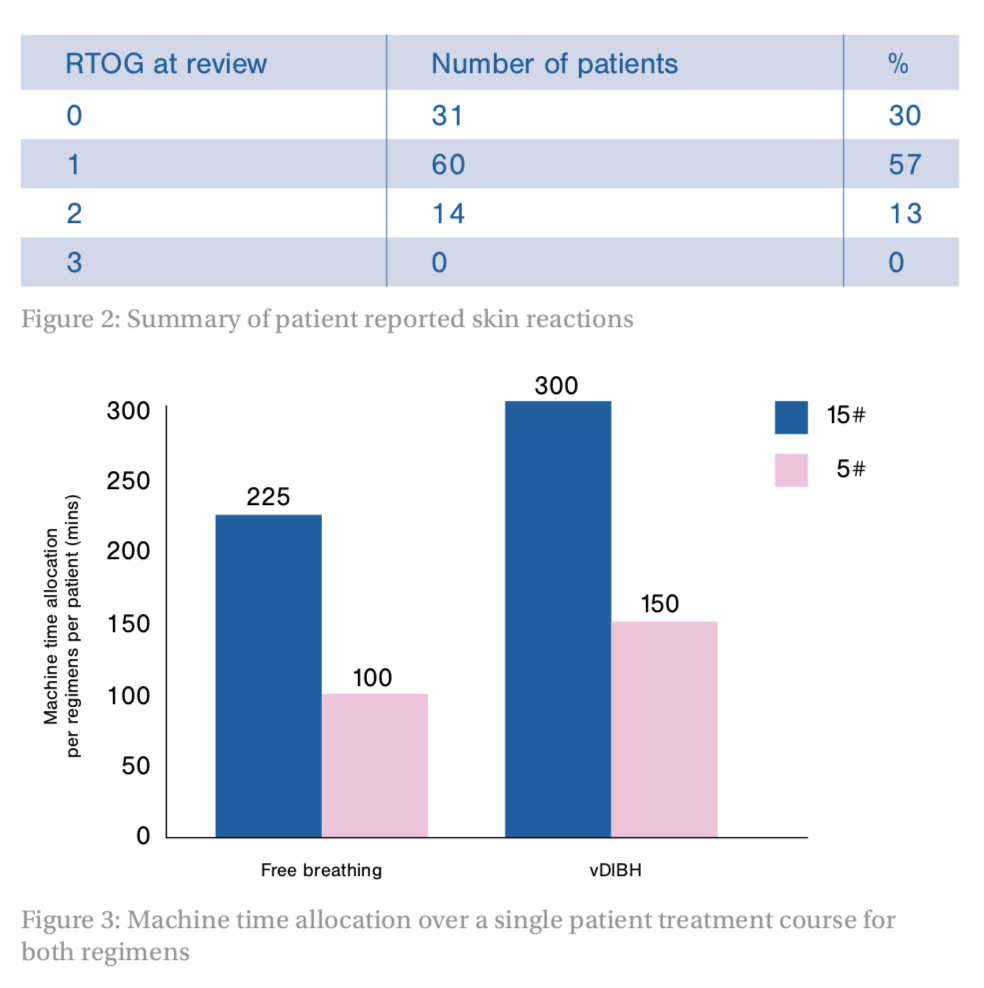
The information recorded in these forms by the nurses gave us a novel set of data to be able to look at skin reactions in this group of patients. It also meant that once enough data was collected, the need for the implemented follow-up telephone call could be evaluated. Figure 2 (below) shows the reported RTOG value at the time of this call for the first 105 patients, with the largest number of patients reporting a value of one, which is comparable to the Fast Forward Trial data4.
From these telephone calls, the patients reporting an RTOG of 2 or above were told to contact the review clinic if their skin began to break down, and one patient was referred for dressings. There were 13 who required further telephone contact with the nurses, four patients who contacted the department themselves and nine who were flagged as higher risk during the initial call and then contacted at a later date by the nurses. Of these 13, nine patients required intervention, which meant a physical appointment either at clinic or with their own GP.
Of all 105 patients treated with this new fractionation (from 7 May to 1 October), only one patient needed physical intervention from the follow-up call, and the audit results were used to prove that these additional telephone calls were not necessary going forward.
All patients receive an ‘end of treatment’ telephone appointment during their final week of treatment. In this, a radiographer details the side effects to be expected once treatment has completed, gives skin care advice and ensures the patient has the relevant contact details should they need further assistance.
It was proposed that the patient advice given during this appointment, together with the departmental Skin Care After Your Radiotherapyleaflet, which all patients receive, covered all the information relevant to this patient group. Patients are encouraged to contact the review clinic should they have any problems with their skin. Encouragingly, the data from the audit shows patients are doing this.
The initial intention was to also use this data alongside another audit completed in the department to produce recommendations on which patients could be identified as at high risk of a significant skin reaction. The other study5 recorded IMF (inframammary fold) measurement and bra size for a group of patients receiving 40Gy in 15 fractions. It found a significant correlation between the severity of the skin reaction and a larger breast size.
However, a comparative analysis using the hypo fractionated patients was not possible with any numerical power because many of the assessments were, unfortunately, not completed fully.
Work continues in the department, looking at how patients at high risk of developing a significant skin reaction can be identified, not just for this patient group but for all patients. These patients need to be identified at the start of treatment rather than at a follow-up post-treatment.
Machine capacity
As well as reducing hospital visits, the other benefit of hypo fractionated treatment is that the machine capacity required for these patients is reduced. At the start of the pandemic, it was unknown how staffing would be affected, either by staff illness or self-isolation. The closure of some of the treatment machines could have been the result if the department was severely affected.
Figure 3 (below) highlights that, despite increasing slot allocation to allow for daily imaging, the five fraction regimen provides a huge saving in machine time – at least two five fraction patients can be treated in the same allotted time as one 15 fraction patient. The radiotherapy department was incredibly fortunate that staffing was not severely affected and the service was able to continue as normal. However, the introduction of the five fraction breast patients also provided a buffer during an uncertain time.
Conclusion
The publication of the Fast Forward Trial five-year results during a global pandemic provided the push needed to implement the hypo fractionated regime of 26Gy in five fractions for breast patients. It provided the opportunity to reduce hospital visits and, therefore, minimise the potential exposure to Covid-19 while maintaining oncological outcome.
A full multidisciplinary team approach was needed to ensure the safe introduction of the new technique, with all aspects of the treatment pathway being assessed and evaluated before implementation. The speed of this implementation in an NHS department which, under normal circumstances, would have taken months, is a credit to all the staff involved: radiographers, physicists, nurses, clinicians, dosimetrists and coordinators. It is hoped that these lessons learned in efficiency can continue post-pandemic.
Figure 1: Summary of protocol changes required
Planning
As Leeds had been a part of the Fast Forward Trial, the same clinical goals for target volume and organs at risk were used as for the initial study.
Verification
Due to the higher dose per fraction, the imaging frequency was changed to daily online imaging.
Treatment delivery
Treatment delivery was no different to standard.
Treatment review
Telephone review 10 days post treatment.
Figure 4: Summary of treatment slot allocation
Treatment booking
The daily slot length accounted for daily online imaging and personal protective equipment (PPE) time:
- Free breathing: 20 minutes
- vDIBH: 30 minutes
A time audit of the first 20 hypo fractionated patients confirmed slot length had been allocated correctly:
- Free breathing: 18.6 minutes
- vDIBH: 26.3 minutes
Figures 2 and 3:
Julie Wood and Helen Dring are advanced practitioners in radiotherapy at Leeds Cancer Centre, St James’s University Hospital, Leeds
References
1.What’s happened to cancer services during the COVID-19 pandemic, Cancer Research UK, viewed December 2020 <www.cancerresearchuk.org>
2.Brunt AM, Haviland JS, Wheatley DA et al. Hypofractionated breast radiotherapy for 1 week versus 3 weeks (FAST-Forward): 5-year efficacy and late normal tissues effect results from a multicentre, non-inferiority, randomised, phase 3 trial. Lancet 2020; 395; 1613-1626
3.Treatment of Radiotherapy Induced Acute Skin Reactions. A clinical guide recommended for use of the College of Radiographers (2000)
4.Brunt AM, Wheatley D, Yarnold J et al. Acute skin toxicity associated with a 1-week schedule of whole breast radiotherapy compared with a standard 3-week regimen delivered in the UK FAST-Forward trial, phase 3 trial. Radiotherapy and Oncology 2016; 120; 114-118
5.Southworth A, Clough H, Roberts N. An Audit of the radiation-induced skin reactions in the inframammary fold; does breast size impact on the severity of the reaction? Radiography 2020; 26; 192-197